Heart attacks and strokes occur when blood flow to the heart or brain is abruptly obstructed, depriving these vital organs of the oxygen and nutrients they require. In most cases, the underlying cause is the accumulation of cholesterol and other substances within the arteries, which can narrow the vessels and lead to the formation of blood clots.
Over time, conditions such as high blood pressure, elevated cholesterol, and diabetes can further damage blood vessels, compounding the risk. Gaining a clear understanding of these causes is critical to effective prevention.
This article will help you understand the main causes of these emergencies and explore effective strategies to significantly reduce the risk.
Symptoms of Heart Attack
Symptoms of a heart attack can vary widely from person to person. While some may experience severe and unmistakable signs, others might notice mild discomfort or subtle changes.
Recognizing these symptoms is critical, as seeking prompt medical attention can save lives and reduce heart damage.
- Chest Discomfort: It is the most common symptom of a heart attack. It may feel like pressure, tightness, heaviness, or a squeezing sensation in the center or left side of the chest. The discomfort can last for several minutes, come and go, or gradually worsen, signalling that the heart is not receiving enough blood.
- Pain in Other Areas: Pain can extend beyond the chest to the arms (usually the left, sometimes both), shoulders, neck, jaw, back, or upper abdomen. This happens because nerves in these areas share pathways with the heart, causing pain to be felt in multiple locations.
- Shortness of Breath: Difficulty breathing, with or without chest pain, often due to fluid buildup in the lungs or reduced oxygen supply.
- Nausea or Indigestion: Feeling sick, vomiting, or experiencing heartburn-like discomfort; more common in women.
- Cold Sweats and Lightheadedness: Sudden sweating, dizziness, or fainting as the heart struggles to pump blood.
- Palpitations: Rapid, irregular, or forceful heartbeat caused by reduced blood flow or stress on the heart.
- Intense Anxiety or Sense of Doom: Overwhelming fear or panic, even without chest pain, as the body senses a severe problem.
- Unexplained Fatigue: Sudden tiredness or weakness, sometimes hours or days before a heart attack, more often reported by women.
Symptoms of Stroke
Stroke symptoms can start suddenly and may vary depending on the area of the brain affected. Recognizing them early is vital, as quick action can prevent serious disability or save a life.
- Sudden Weakness or Numbness: Loss of strength or sensation in the face, arm, or leg, usually on one side of the body.
- Difficulty Speaking or Understanding: Slurred speech, trouble finding the right words, or difficulty understanding others.
- Vision Problems: Sudden blurred vision or loss of sight in one or both eyes.
- Severe Headache: A sudden, intense headache, sometimes described as the worst ever experienced.
- Dizziness or Loss of Balance: Trouble walking, feeling unsteady, or losing coordination.
- Facial Drooping: One side of the face may droop, causing an uneven smile.
- Confusion: Feeling disoriented or having trouble following simple instructions.
- Nausea or Vomiting: May accompany other stroke symptoms, especially if the brainstem is involved.
Causes of Heart Attack
A heart attack can occur for several reasons, all of which interfere with the blood supply to the heart. Understanding these causes helps in recognizing risk factors and taking preventive steps. The major causes are outlined below:
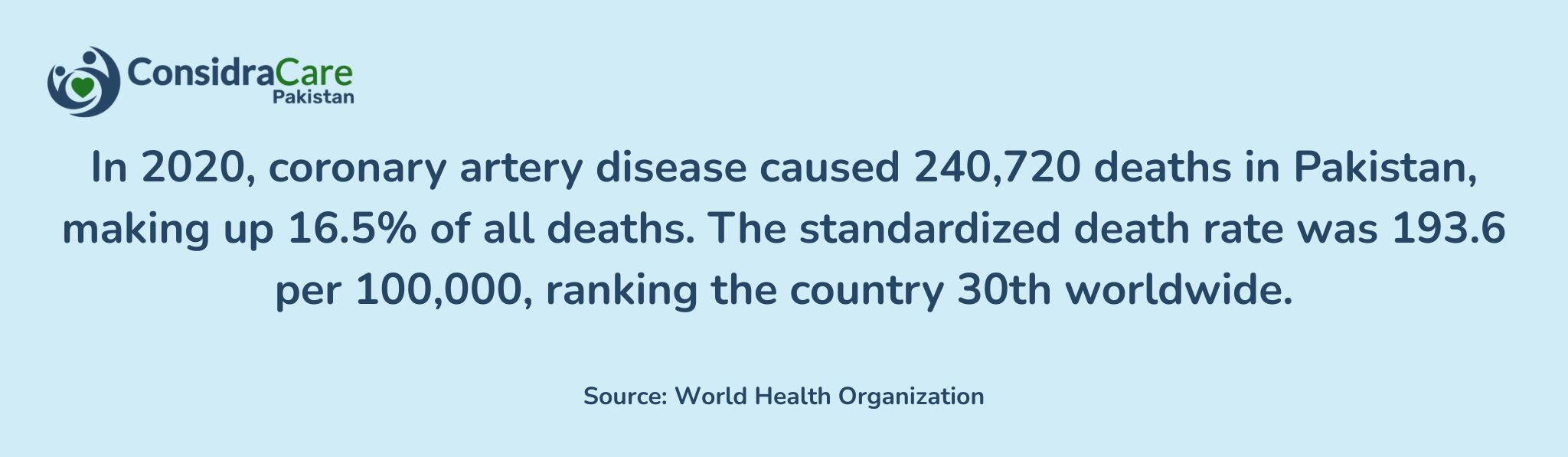
1. Coronary Artery Disease (CAD):
Most heart attacks result from coronary artery disease, a condition in which one or more coronary arteries become narrowed or blocked. This narrowing is usually caused by the buildup of cholesterol, fats, calcium, and other substances, forming plaques along the artery walls. These plaques reduce blood flow to the heart, and if one ruptures, a blood clot can form, completely blocking the artery and triggering a heart attack.
2. Plaque Rupture:
Plaques may be stable or unstable. When the outer layer of a plaque cracks, blood platelets gather at the site, forming a clot that can obstruct blood flow. As a result, the heart muscle is deprived of oxygen, causing cells to die and leading to permanent damage.
3. Heart Muscle Damage:
The severity of damage depends on which artery is blocked and how long the heart is without blood. Healing begins over the following weeks, forming scar tissue in the affected area. Unlike healthy heart muscle, scar tissue cannot contract efficiently, which may reduce the heart’s pumping ability.
4. Complete vs. Partial Blockages:
A complete blockage in a medium or large coronary artery typically causes a severe heart attack known as ST-elevation myocardial infarction (STEMI).
A partial blockage usually results in a non-ST-elevation myocardial infarction (NSTEMI), although some NSTEMI cases involve a total blockage.
5. Coronary Artery Spasm:
A sudden, severe tightening of a coronary artery, called a coronary artery spasm, can reduce or stop blood flow even if there is little or no plaque. This condition, also known as Prinzmetal’s angina or vasospastic angina, is more likely in individuals who smoke or have early signs of artery stiffening. Certain drugs, such as cocaine, can also trigger spasms.
6. Spontaneous Coronary Artery Dissection (SCAD):
SCAD is a rare but serious condition in which a tear forms within a coronary artery. Blood clots or the torn tissue itself can block the artery, causing a heart attack. This condition is more common in women under 50, pregnant women, and individuals with connective tissue disorders such as Marfan syndrome.
7. Coronary Artery Embolism:
A coronary artery embolism occurs when a clot or other obstruction travels through the bloodstream and lodges in a coronary artery, blocking blood flow to the heart muscle. People with atrial fibrillation or other clotting disorders are at higher risk.
8. Other Causes:
Heart attacks can also arise from artery tears, congenital artery abnormalities, viral infections such as COVID-19, or severe drops in blood pressure and oxygen levels.
Causes of Stroke
A stroke can occur due to various conditions that block or reduce blood flow to the brain. Understanding these causes is essential for prevention and early intervention. The main causes are as follows:
1. Ischemic Stroke (Blocked Arteries):
This is the most common type of stroke. It occurs when fatty deposits (plaques) or blood clots obstruct the arteries that supply blood to the brain, cutting off oxygen and vital nutrients.
2. Hemorrhagic Stroke (Burst Blood Vessel):
A hemorrhagic stroke happens when a weakened blood vessel in the brain ruptures, causing bleeding inside or around the brain. High blood pressure, aneurysms, or excessive use of blood-thinning medications can trigger this type of stroke.

3. Transient Ischemic Attack (Mini-Stroke):
Also known as a warning stroke, a Transient Ischemic Attack (TIA) occurs when blood flow to the brain is temporarily blocked. Although symptoms resolve quickly, a TIA is a serious indicator that a full stroke may occur in the future.
4. Blood Clots and Embolisms:
Blood clots can form in other parts of the body, such as the heart, and travel to the brain. Atrial fibrillation, an irregular heartbeat, is a common cause of these clots and increases stroke risk.
5. Narrowed Arteries (Atherosclerosis):
Plaque buildup inside the arteries can narrow them, restricting blood flow to the brain and raising the likelihood of a stroke.
6. Additional Causes:
Other conditions that can lead to stroke include brain aneurysms, head injuries, certain genetic disorders, and medical conditions that affect blood clotting.
Risk Factors for Heart Attack and Stroke
Certain lifestyle choices and health conditions can increase the likelihood of a heart attack or stroke by gradually damaging the heart and blood vessels:
- High Blood Pressure: It is a leading contributor to both heart attack and stroke. It strains the heart, weakens arteries in the brain, and damages blood vessels throughout the body.
- High Cholesterol: Promotes fatty deposits in arteries that supply the heart and brain, potentially blocking blood flow and increasing the risk of cardiovascular events.
- Smoking: Damages blood vessels, thickens the blood, and reduces oxygen levels, significantly raising the risk of heart attack and stroke.
- Diabetes: Can impair blood vessels, slow circulation, and accelerate plaque buildup, heightening the chances of both heart attack and stroke.
- Obesity and Unhealthy Diet: Excess weight and poor nutrition can elevate blood pressure and cholesterol, placing additional strain on the heart and increasing stroke risk.
- Physical Inactivity: An inactive lifestyle weakens the heart, slows healthy blood flow, and contributes to weight gain, all of which increase the risk of cardiovascular problems.
- Family History: Genetic predisposition to heart disease or stroke increases an individual’s risk.
- Age and Gender: Risk rises with age. Men are more prone to early heart issues, while women’s risk increases after menopause, and they face a higher likelihood of stroke-related death.
- Stress and Excessive Alcohol: Chronic stress and heavy drinking can raise blood pressure, provoke irregular heart rhythms, and damage arteries over time.
How to Prevent Heart Attacks?
Preventing a heart attack requires adopting heart-healthy habits and managing conditions that put stress on the heart. Effective steps include:
- Eat a Balanced Diet: Focus on fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated fats, excess salt, and sugary foods that contribute to plaque buildup.
- Stay Physically Active: Regular exercise strengthens the heart and improves circulation. Aim for at least 30 minutes of moderate activity, such as walking, swimming, or cycling, most days of the week.
- Maintain a Healthy Weight: Carrying excess weight increases the risk of high blood pressure, high cholesterol, and diabetes, all of which strain the heart.
- Quit Smoking: Tobacco damages blood vessels, reduces oxygen supply, and accelerates atherosclerosis. Quitting smoking significantly lowers the risk of a heart attack.
- Manage Stress: Chronic stress can elevate blood pressure and encourage unhealthy habits. Practices like deep breathing, meditation, or prayer can help reduce stress.
- Control Health Conditions: Keep blood pressure, cholesterol, and diabetes under control with regular checkups, medications if needed, and lifestyle adjustments.
- Limit Alcohol Intake: Excessive drinking raises blood pressure and harms the heart. If consumed, alcohol should be limited and taken in moderation.
- Follow Medical Advice: Take prescribed medications consistently and attend scheduled checkups to detect and manage any emerging heart issues early.

Preventions for Stroke?
Stroke prevention emphasizes maintaining healthy blood vessels and ensuring uninterrupted blood flow to the brain. Key steps include:
- Keep Blood Pressure Under Control: High blood pressure is the leading risk factor for stroke. Regular monitoring, limiting salt intake, and taking prescribed medications can help maintain healthy levels.
- Manage Blood Sugar Levels: Diabetes can damage blood vessels and increase stroke risk. A balanced diet, regular exercise, and proper medication can help keep blood sugar in check.
- Monitor Cholesterol Levels: Excess cholesterol can block arteries supplying the brain. Eat a diet low in unhealthy fats and follow medical guidance if cholesterol-lowering medications are needed.
- Address Heart Rhythm Issues: Irregular heart rhythms, especially atrial fibrillation, can cause blood clots that travel to the brain. Early detection and treatment significantly reduce stroke risk.
- Manage Stress and Sleep: Chronic stress and poor sleep can elevate blood pressure and harm overall cardiovascular health. Healthy routines, relaxation techniques, and adequate rest support brain and heart protection.
Treatment for Heart Attack
Immediate treatment for a heart attack is crucial to preserve heart muscle and minimize long-term damage. The approach depends on the severity of the blockage and how quickly medical care is received.
1. Emergency Care:
- Medical Help: Call emergency services as soon as symptoms appear. Rapid intervention can save lives and reduce heart damage.
- Oxygen and Aspirin: Oxygen may be administered, and aspirin is often used to thin the blood and prevent further clotting.
2. Medications:
- Clot-Dissolving Drugs (Thrombolytics): Help dissolve blood clots obstructing the arteries.
- Blood Thinners: Drugs like heparin or antiplatelet medications prevent new clots from forming.
- Beta-Blockers and ACE Inhibitors: Reduce strain on the heart and improve survival rates.
- Statins: Lower cholesterol levels and help prevent future blockages.
3. Procedures:
- Angioplasty and Stenting: A balloon is used to open blocked arteries, and a stent is placed to keep them open.
- Bypass Surgery (CABG): Surgeons create an alternate pathway for blood flow around blocked arteries, restoring proper circulation.
Treatment for Stroke
1. Emergency Care:
- Rapid Response:
- Clot-Dissolving Medication (tPA): For ischemic strokes, Tissue Plasminogen Activator (tPA) can dissolve clots if administered within a few hours of symptom onset.
2. Medications:
- Antiplatelet (e.g., Aspirin): Helps prevent new clots from forming.
- Anticoagulants (e.g., Warfarin): Used for patients with atrial fibrillation or other clotting disorders.
- Blood Pressure and Cholesterol Medicines: Manage underlying risk factors that contribute to stroke.
3. Procedures:
- Mechanical Thrombectomy: A procedure to remove a clot from a brain artery, typically performed within a specific time window.
- Surgery: For hemorrhagic strokes, surgery may be necessary to repair damaged blood vessels or relieve pressure on the brain.
4. Rehabilitation:
- Physiotherapy and Speech Therapy: Support recovery of movement, coordination, and communication skills.
- Occupational Therapy: Helps patients regain independence in daily activities and adapt to any long-term limitations.
Read More: How Home Care Services are Changing Rehabilitation in Pakistan?
Protecting Your Health with ConsidraCare
Our team provides expert guidance, personalized care plans, and ongoing support to help prevent, manage, and recover from heart attacks and strokes.
From lifestyle advice and regular health monitoring to emergency preparedness, we are committed to keeping you and your loved ones safe and healthy.
Conclusion:
Heart attacks and strokes are serious, life-threatening conditions, but many cases can be prevented or managed with timely action and healthy habits.
By adopting a balanced diet, staying active, or managing stress, you can significantly reduce the risk of these emergencies.
FAQs
1. What is the main cause of heart attacks and strokes?
2. What are the key warning signs of a stroke?